Sex, gender and medical data: a way forward
Susan Bewley, Margaret McCartney, Catherine Meads and Amy Rogers published an article in the British Medical Journal calling for clarity about sex and gender in medical records and data.
This “rapid response” from Sex Matters co-founder Maya Forstater was published online by the BMJ.
Thank you for publishing this article which raises important issues about data integrity and protection around the attribute “sex” in NHS data systems.
As the authors state “Sex and gender are not synonymous.” Sex, relates to biology – male or female. This is a fact about a person which is observed at birth (in most cases without ambiguity or difficulty) and recorded, in a binary fashion into a baby’s NHS number and their medical record. This fact about a person that does not change. However these records are now corrupted.
Gender can mean a number of different things which are not consistent or synonymous with each other
| 1. A synonym for sex | |
| 2. The broad patterns of behaviour and appearance of the two sexes | |
| 3. Appearance/perception | i) The clothing and appearance norms associated with either sex ii) Being perceived as a particular sex iii) Wishing to be perceived as a particular sex iv) Making an effort through appearance to appear as a particular sex |
| 4. Social roles | i) The traditional social roles and expectations of behaviour of the sexes ii) Wishing to be treated as a particular sex iii) The extent to which someone conforms to traditional social roles |
| 5. Self expression/identity | i) A means of self- expression ii) An internal feeling of being a particular “‘gender’” (or both or neither) |
| 6. Language | i)The words used to refer people by sex (e.g. him/her, Mr, Ms) ii)The words a person uses to refer to themself iii)The words a person wishes other people to use to refer to them iv) The words other people spontaneously use to refer to someone |
Basic principles of data management are that each field or attribute should be clearly defined and contain only that information. Healthcare providers and the NHS should hold accurate, reliable information about patient’s sex as a basic minimum.
At the moment they do not. There is no single data attribute that records that I am female (and not in fact a male person who identifies as female and has asked to have their record changed).
More than ten years ago the NHS recognised the need for clear systems for recording biological sex and making sure it was not conflated with social gender. They carefully set up a system of data and definitions which could deal with both.
The data standard for the User Interface, written in 2009, explained:
The term ‘Gender’ is now considered too ambiguous to be desirable or safe…
The data standard set out definitions for patient “sex” and “current gender” and warned:
Users may confuse the terms current gender and sex, or assume that they are synonymous. Therefore, it is essential that all NHS applications display and explain current gender and sex terminology and values in a clear and consistent manner.
The policy set out in detail how to keep these two characteristics separate and unconfused, and how to design computer interfaces to ensure that sex data was captured (with social gender as an optional extra). It also set out potential consequences of not adhering to these standards including:
- The patient is given the wrong treatment as a result of a failure to identify the patient correctly.
- The patient is given the wrong treatment as a result of a failure to match the patient correctly with their artefacts (samples, letters, specimens, X-rays, and so on).
- The patient is given the wrong treatment as a result of a failure in communication between staff, or staff not performing or checking procedures correctly.
- The patient is categorised with a value that cannot be utilised by any other systems.
- The patient is categorised incorrectly from a legal perspective.
- The patient is categorised incorrectly from their perspective.
However despite establishing the basis for meeting these principles this system was not implemented. The current NHS data dictionary differentiates, “phenotypic sex” (as observed by a clinician) and “patient stated gender”, but in practice “male” and “female” are recorded only against gender and the phenotypic sex field typically remains empty.
Policies to allow patients to change their registered “gender” are now embedded across the NHS
The GMC tells doctors to change a patient’s sex/gender as recorded on medical records on request. This does not require any medical diagnosis, anatomical changes or a legal gender recognition certificate.
Public Health England tells GP surgeries to change a patient’s’ recorded sex/gender on their medical record at any time, without requiring diagnosis or any form of gender reassignment treatment. They are given a new NHS number and previous medical information must be “gender neutralised” and transferred into a newly created medical record. They will be sent screening appointments (e.g. for cervical smear tests or prostate cancer screen) according to their new gender (i.e. invitations to attend the wrong screenings).
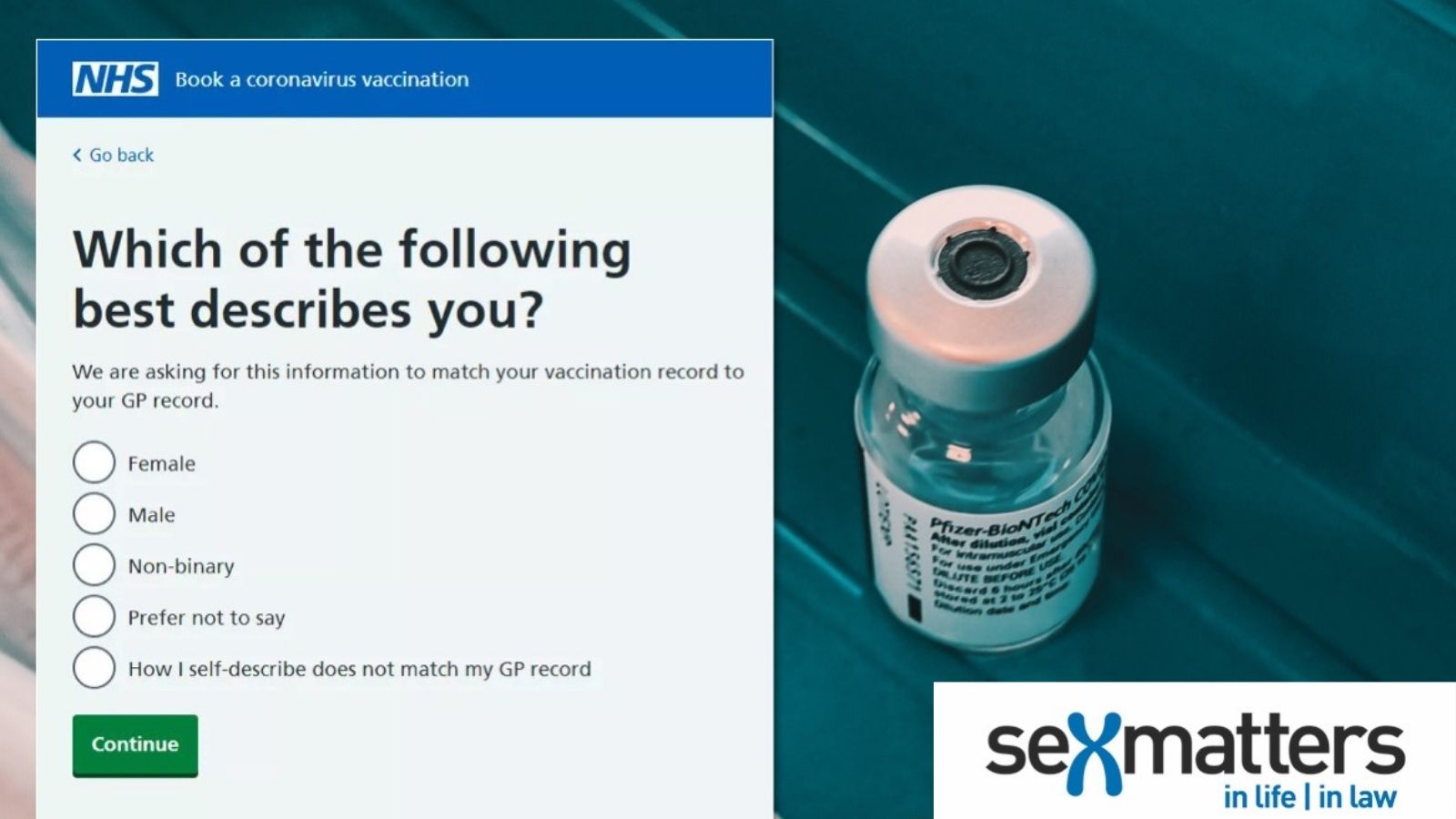
Gender (self identified as male or female) is held by the Patient Demographic Service (PDS) for matching rather than clinical purposes. But it has recently been removed from the API because of sensitivity of people who identify as non binary and do not wish to be identified by their sex.
This approach shows the way forward
Sex should not be confused with gender identity, or any other of the myriad definitions of gender. Accurate information on everybody’s sex should be held in their NHS record but it should only be disclosed or displayed when it is needed and should not be used for matching purposes.
The authors state that “sex and gender should not be used interchangeably”. In fact data quality risks mean that “gender” should not be used as an attribute at all, because it is undefined and invites confusion.
Aspects of social gender such as titles, name used, and preferred pronouns can be recorded in other fields to facilitate social interaction. Transgender identity may be recorded.
Given that the law allows people to change their legal sex, a field may be needed where people’s legal sex is recorded, without changing the record of their biological sex (since this, in fact, has not changed and it destroys day integrity for everyone if the field can contain either biological or legal sex).
If someone has a diagnosis or medical treatment such as hormones or surgery to change the appearance of their sex, this of course should be in their medical record.
Greater clarity about definitions, privacy, confidentiality and data protection would allow people to keep their sex private in situations where it is no one else’s business but maintain the integrity of medical records. In NHS systems this would need to include a general system of not displaying the last digit of NHS numbers on screen.
Data protection principles apply to everybody and currently the NHS (along with the Passport Office and DVLA) are failing in these principles by requiring information about individual’s sex, but then processing it in such as way (mixing it in a category with self declared gender) that the data is corrupted.
As the ONS case over the census highlighted by the authors shows, there will be legal challenges. The Digital Identities Trust Framework being developed by DCMS is also an opportunity to fix the problem of data corruption of the sex attribute.
The NHS should establish a task force to understand the corruption of sex data across medical records and establish a plan to fix it.
Rapid responses are electronic comments to the editor. They enable BMJ users to debate issues raised in articles published on bmj.com. Rapid responses are not indexed in PubMed and they are not journal articles.
